Hope & Health
Articles and Updates from WVU Medicine Golisano Children's
09/5/2025 | Maria Khan, PhD, and Jessica Marcrum, PsyM
Child Trauma: Busting Myths for Better Care
Trauma isn’t just a negative or uncomfortable experience. Trauma is the result of experiencing or witnessing something dangerous or scary that threatens safety and has a lasting impact on one’s well-being. A traumatic event is often unpredictable and can be described as something that should not have occurred.
Children are vulnerable to all sorts of traumatic or adverse childhood experiences (ACEs), including but not limited to:
- Abuse and neglect
- Exposure to violence
- Exposure to substance use
- Major accidents
- Medical procedures and hospitalizations
- Bullying
- Separation or loss of loved ones
- In-utero exposures before birth
When a child is exposed to multiple traumatic events with long-term effects, this is called complex trauma. Typically, complex trauma involves early abuse and neglect, which affects child development and social, emotional, and behavioral functioning. Children who experience trauma, especially complex trauma, are significantly more likely to have future anxiety, depression, developmental and academic difficulties, substance use, and health problems.
How common is child trauma? Contrary to what most would like to believe, child trauma is common. About 60 percent of youth in the U.S. experience one or more traumatic events by the age of 17. In the U.S., 7.4 per 1,000 children (i.e., over 500,000 children) experience abuse and neglect annually. Most children are abused by a known and trusted adult, and younger children are the most vulnerable. Unfortunately, West Virginia has the highest rate of Child Protective Services (CPS) investigations per capita, and one third of abused or neglected children in West Virginia had substance-involved caregivers.
Notably, these numbers represent cases that were reported and investigated by CPS. Unfortunately, countless children experience traumatic events that may go unrecognized, unreported, and unaddressed.
What is traumatic stress? Following trauma exposure(s), children may exhibit wide-ranging emotional and behavioral reactions called “traumatic stress.” Certain risk factors may increase the chance of developing traumatic stress (e.g., severity and chronicity of trauma, closeness of perpetrator, age, caregiver reactions). Common traumatic stress symptoms include:
- Re-experiencing the trauma through intrusive memories, dreams, or flashbacks
- Avoiding physical reminders of the trauma or thoughts/feelings/memories of the trauma
- Negative thoughts and feelings, such as self-blame, low mood, low interest, withdrawal
- Physical reactions, including sleep problems, outbursts, concentration difficulties, being on edge, becoming easily startled
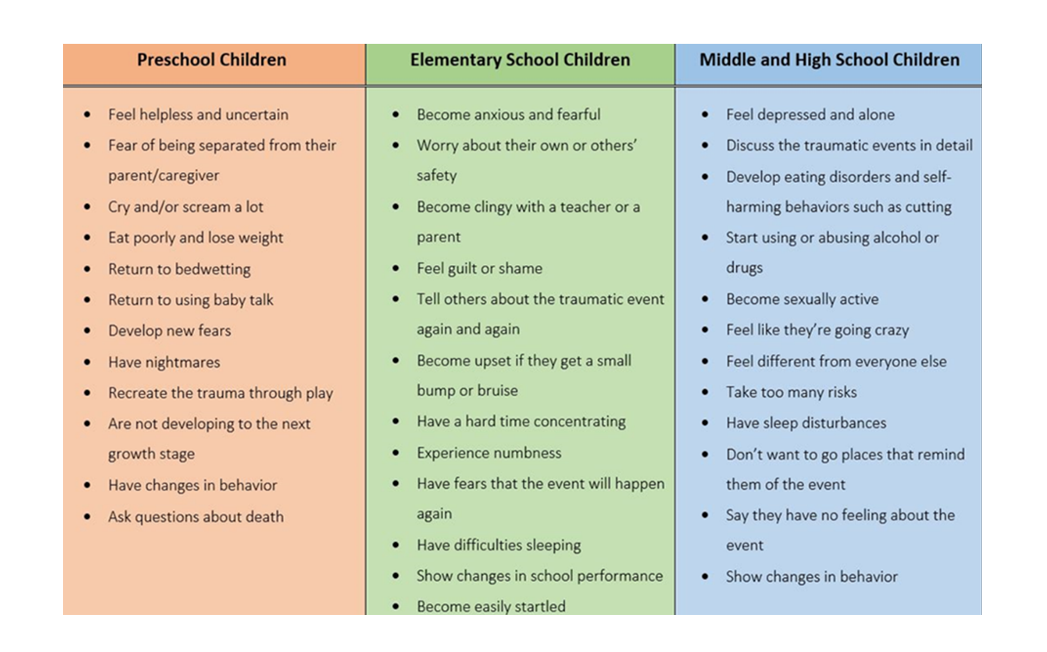
Children may display different signs of traumatic stress, depending on age and developmental stage. The National Child Traumatic Stress Network provides copious resources to help providers and parents better recognize the signs of potential traumatic stress:
Although it’s tough to diagnose, young children certainly can have post-traumatic stress disorder (PTSD) or another trauma/stressor disorder. Just as important as recognizing potential warning signs is understanding that not all children who experience trauma will develop traumatic stress.
Myths about trauma:
- Talking or asking about trauma makes things worse.
- If you endure trauma, you will have PTSD.
- Children are young, so they “get over it.”
- Everyone who has been through trauma needs therapy.
- Experiencing trauma means something is wrong with you.
How to be more trauma informed (no matter who you are) Given that West Virginia has some of the highest rates of child trauma nationally, it’s up to all of us to better recognize how to help children undergoing difficult experiences. Talking about trauma is hard, and many caregivers fear bringing it up could make children feel upset or unsafe.
However, the most important thing for children who have experienced traumatic events is support from loved ones. Children who feel heard, believed, and connected to safe adults have fewer traumatic stress difficulties than those who feel alone in their experiences. Some tips to consider for children who experienced trauma:
- Establish a daily routine – This provides predictability, which is calming.
- Support and listen to children – This helps children feel connected and less alone.
- Help build self-regulation – Help children with breaks and “calm down” activities.
- Lead with empathy – Try to put yourself in your child’s shoes and not judge.
- Provide encouragement – Help your child feel they are working hard and succeeding.
Seek help if needed If you’re concerned about your child or family, we encourage you to reach out to your medical providers or directly to our clinic. The Resilience After Complex Trauma (ReACT) Clinic within the WVU Medicine Behavioral Medicine and Psychiatry Program specializes in treating children, parents, and families dealing with traumatic exposures and/or traumatic stress.
References *Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine, 14(4), 245-258.
Finkelhor, D., Turner, H. A., Shattuck, A., & Hamby, S. L. (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the national survey of children’s exposure to violence. JAMA pediatrics, 169(8), 746-754.
Hogg, B., Gardoki-Souto, I., Valiente-Gómez, A., Rosa, A. R., Fortea, L., Radua, J., … & Moreno-Alcázar, A. (2023). Psychological trauma as a transdiagnostic risk factor for mental disorder: an umbrella meta-analysis. European Archives of Psychiatry and Clinical Neuroscience, 273(2), 397-410.
The National Child Traumatic Stress Network (2025). https://www.nctsn.org/resources/all-nctsn-resources
U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. (2025). Child Maltreatment 2023. Available from https://www.acf.hhs.gov/cb/data-research/child-maltreatment.*
